
The Cost of Doing Nothing
Assessing the Value of Upgrading Pneumatic Tube Systems
Where You'll Find the Costs
Hospital systems of all sizes struggle with the cost of updating legacy infrastructure that isn’t “broken.” With facilities managers who respond quickly to alerts or downtime, the effects of poor system performance can go unnoticed by executive leadership and, therefore, are not a priority during budgeting.
Instead of optimizing and upgrading a pneumatic tube system to improve throughput, security, and turnaround times, hospitals often fall into these two categories:
1. Creating transportation workarounds to maintain the status quo
If an organization does not want to invest in upgrades to their tube system hardware and software, they will continue to experience degradation in productivity over time. This creates distrust among the users who depend on the system for the delivery of medications and lab samples. An increase in downtime also causes a need for additional courier staff or, worse, manual transport by skilled clinical or nursing professionals. This creates a slow, error-prone process that is full of waste and, therefore, added costs. Every additional human touch can lead to inefficiencies and opportunities for error.
2. Choosing to invest in patient-facing projects instead of hospital infrastructure
Like most companies, hospitals typically invest in the front end of their business before the back end. Clinical areas often receive most of the money available for capital investment while facilities and materials management are viewed purely as expenses. To improve service for patients and and support for clinical staff, hospitals should consider investing in upgrades to key infrastructure. Tube systems are just one part of a hospital’s key infrastructure on which available funds should be deployed to ensure the delivery of clinical and support services.Three Approaches for Evaluating Tube System Optimization
Approach One: Do Nothing
In a true do-nothing scenario, there are no upgrades to intuitive touchscreen panels, no security or tracking improvements, and no enhancements to communication lines or vintage hardware. In this approach, hospital leadership expects facilities managers to make do with what they have.
When executives are only looking at short term financials, they do not always see the long-term and relative costs of doing nothing. Among them are incremental costs, which can rise when doing nothing, for many reasons:
- There is an increased need for spare parts so that replacements can be made quickly in a time of failure and the system can return to operation.
- Additional staffing is required to deliver medications and lab samples when the pneumatic tube system is down. Often this means nurses and pharmacy technicians are doing manual labor instead of focusing on patient-facing activities, such as medication reconciliation and administration.
- Without tube system delivery available, nurses spend extra time searching for missing medications and calling the pharmacy. This time away from patients can have costly implications for quality scores.
- Calls from nursing to pharmacy cause interruptions and distractions. Research shows that distractions contribute to 45% of medication errors in hospitals
and health systems.1 The safety, financial and reputation implications of these errors pose a major risk for hospitals.
Approach Two: Partially Upgrade, Minimize Greatest Risks
Upgrading a pneumatic tube system can mean a wide range of improvements, with varying investments. When considering a modernization project, it’s important to begin with a system health audit. Engage your tube system vendor or choice for a consultation to determine your most urgent needs based on current system performance. Premium providers will be able to consult on your total system and possibilities, no matter which company is your current provider. By benchmarking your system against other high-performing facilities, you can develop a roadmap to achieving your goals. To accommodate budget constraints, this can be accomplished with a phased approach of upgrading small portions of the system at a time.
For facilities who choose to partially upgrade there are two common approaches:
1. Upgrade obsolete or aging technology
Evolving market needs, including increasing legislative pressures, have led to innovations in automated delivery, such as improved traceability and security. With the development of new hardware and software, older systems become out-of-date and unable to support the features needed by end users. As your tube system vendor communicates plans to sunset these parts, take the opportunity to evaluate your current state. Does it make sense to upgrade immediately, or should you invest in extra safety stock of replacement parts and budget for a future upgrade? Your vendor can help guide you in determining the best course of action.
By beginning your tube system modernization initiative with addressing obsolete technology, you can avoid significant downtime. Replacement parts for current versions are always available and your upgraded technology will be fully supported by your vendor partner.
2. Upgrade the software backbone of the system
At the heart of every tube system is the software that orchestrates material movement, ensuring intuitive routing, traffic management, security and traceability. Today’s rapidly evolving technology landscape demands that your tube system software meet enhanced IT and security requirements. As these change frequently, forward-thinking vendors are moving to a software subscription model that ensures your system is always running on the current version. In the new model, bug fixes and feature developments are pushed proactively, helping you avoid downtime and provide security against cyber-attacks.
By beginning your tube system modernization initiative with an upgrade to the latest software, you set yourself up for success with additional projects. Whether you plan to upgrade panels or add on chain-of-custody tracking for medication deliveries, you’ll need, and want, the reliability of the most current software.
When evaluating a partial upgrade to your pneumatic tube system, it’s critical to consider your greatest risks. What is the cost of system failure and which components of your system are most likely to cause downtime? Prioritizing the most important improvements will help in realizing the impact of inaction.
After upgrading our pneumatic tube system communication lines to Ethernet, we experienced improved system uptime, fewer alarms and a reduction in calls from users. Our clinical staff is more satisfied with the performance, which means I spend less time maintaining the system.
Approach Three: Completely Upgrade,
Save Money
“How is this spend justified?”
1. When hospitals delay upgrades, they increase their risk for catastrophic failure. This can lead to costly repairs, such as overnighting parts and emergency technician visits during off hours, and more importantly, unscheduled interruptions to delivery of patient care, impacting their experience and satisfaction scores.
2. When hospital transport systems fail, deliveries don’t arrive on time, pharmacies are distracted, lab tests are slow, nurses waste time searching for medications, medication administration is delayed and patients suffer. This can lead to costly medication errors and poor quality scores, which impact reimbursement, and ultimately, the financial health of your organization.
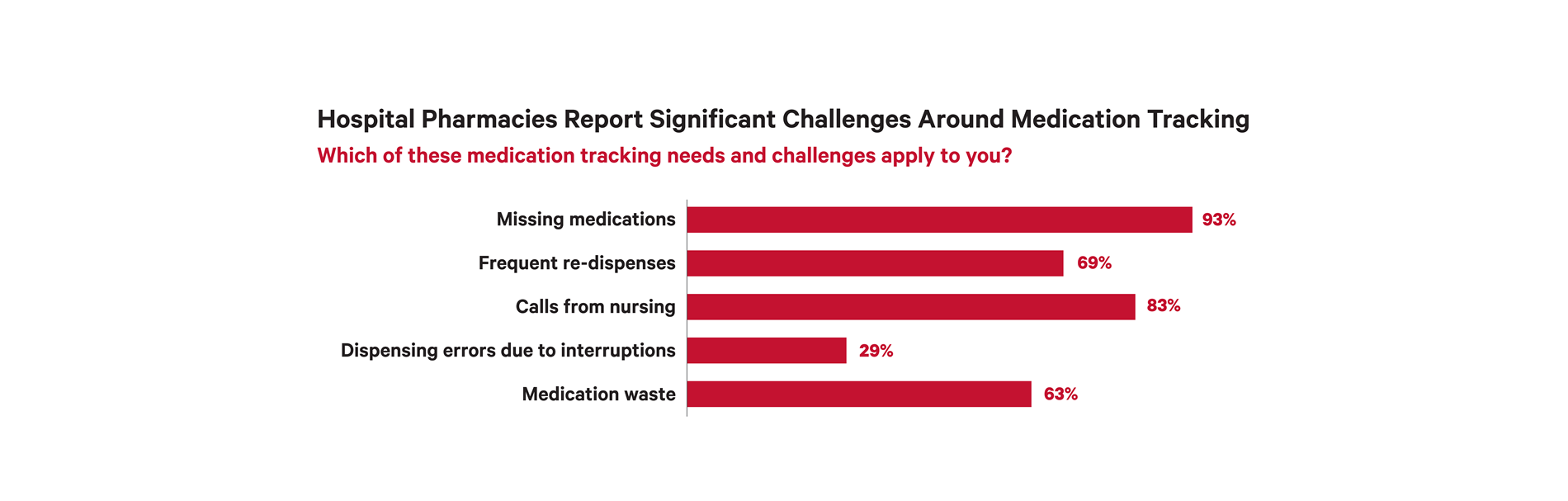
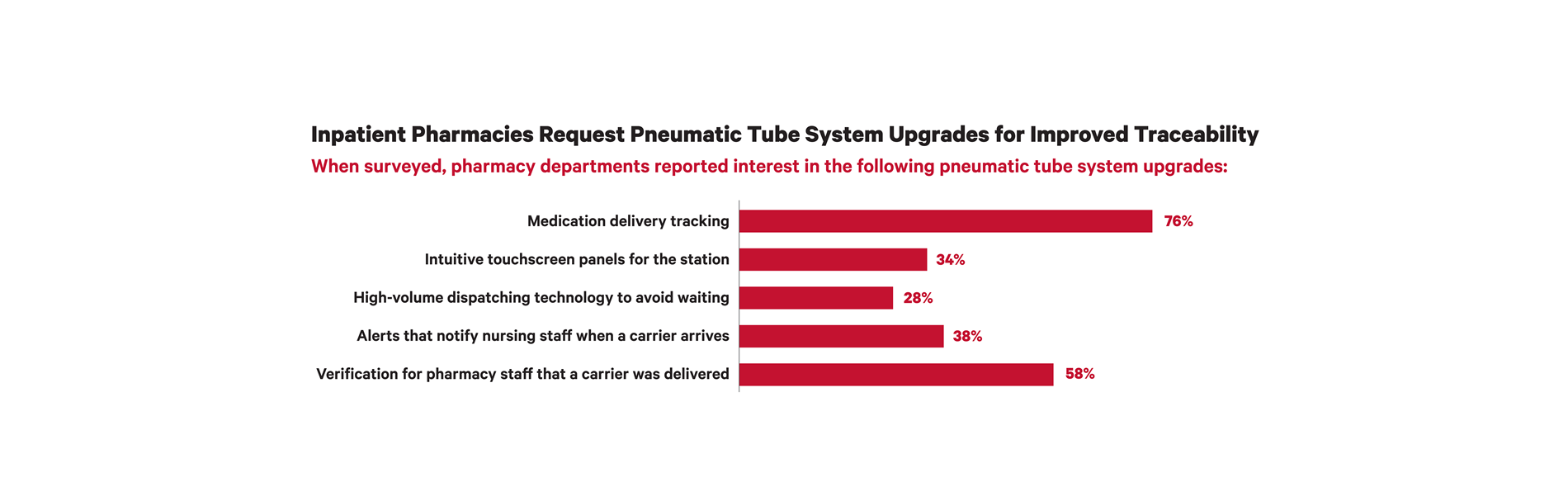
3. Increased medication tracking requirements are putting hospitals at risk for non-compliance. As a critical piece of medication delivery, your tube system must be equipped with technology that supports chain-of-custody needs. The vintage of your hardware and software may prevent you from adding the track-and trace functionality your pharmacy users need. Putting the needs of patients and clinical staff at the center of your capital request will increase the likelihood of approval. See graph below for market research on the tube system upgrades that are prioritized by hospital pharmacies.
Highlighting the cost of doing nothing is critical to gaining approval for a complete upgrade to your tube system. Keep in mind that even if you decide to move forward with a complete upgrade, it can still be implemented in phases, to be minimally disruptive and budget-conscious.
Trends Impacting Medication Delivery Inside Hospitals
Six Critical Challenges from Inaction
1. System Downtime
When a pneumatic tube system experiences downtime, labor is needed to courier those deliveries. Assuming an average of eight transactions per patient bed, there are 2,400 transactions a day at full census for a 300-bed hospital. Research shows that on average, couriers can make 10 deliveries an hour. At a rate of $15 per hour, system downtime would cost $3,600 per day. That means the tube system is saving that facility $1,314,000 annually in direct cost.
2. Lost Opportunities
The same calculation for system downtime can be applied to lost opportunity costs. When a system is no longer seen as reliable by end users, they may stop using it. Information can be gathered by end users to determine what percentage of deliveries they are choosing not to tube. This percentage can be used to calculate labor. Distrust of the system can also impact speed to diagnosis. For example, if a phlebotomist decides they will walk all of their samples back with them to the lab instead of dispatching carriers immediately after they draw, turnaround time is greatly impacted.
3. Medication Errors
Preventable medication errors injure 1,500,000 people each year, costing $3,500,000,000 in unnecessary medical costs.4,5 When nurses call the pharmacy about missing medications due to poor pneumatic tube system performance, they create distractions. The error rate for prescriptions with one or more interruptions is 6.65%.6 This demonstrates how tube system reliability issues can be detrimental to patient safety.
4. Drug Diversion
Drug diversion is a serious concern for many hospitals and a tube system can play a key role in mitigating these risks. When medications are diverted, the pharmacy needs to redispense them, which creates shrinkage and labor waste. It also delays the time it takes for a medication to reach patients, which is related to the quality measurements being used to determine reimbursement to hospitals. A delay in addressing a patient’s pain can have a ripple of negative effects.
5. User Queuing
Slow, inefficient tube systems often lead to labor waste in the form of user queuing. Nurses line up to receive patient orders and pharmacy technicians have to wait to send carriers because the system is tied up. This is inefficient and takes staff away from patient-facing activities. Because patient satisfaction is now a driver of hospital revenue, this queuing could be impacting your bottom line.
6. Obsolete Technology
When a vendor is no longer able to provide replacement parts or support for the hardware or software in your facility, that creates a significant amount of risk. While most companies strive to give at least a year’s notice, there’s no anticipating when this will happen or when it will fall within your budget cycle. While obsolescence is a natural part of every product life cycle, it creates urgency for you to act. If you choose to wait until something goes wrong, you can end up paying more and causing disruptions for clinical staff.
Key Considerations for Determining the Cost of Doing Nothing
Obsolete tube system hardware and software cannot keep up with increasingly complex delivery requirements, for example, track-and-trace regulations. Before these systems fail, hospitals should evaluate the cost of doing nothing, along with options to modernize.
Think of this as a guide to determining the true cost of doing nothing to improve your tube system in comparison with competing investment options in your facility.
Status quo risks identified by answering these questions
- How many medication deliveries will need to be made manually?
- What does system downtime cost in labor waste?
- How will the patient floors receive urgent blood deliveries?
- How will service to patients be impacted?
- What will be the effect on patient satisfaction and outcomes?
- What if there are no replacement parts for outdated hardware?
- How will we meet Drug Supply Chain Security Act (DSCSA) requirements with our current technology?
Benefits of upgrading
- Improve patient outcomes through enhanced logistics
- Reallocate resources to clinical or safety tasks instead of couriering the medications
- Enhanced transaction visibility help meet DSCSA legislation

Evaluating Modernization Options for Your Facility
Whether you choose to complete a partial upgrade, or undergo a large-scale project, you will need to make decisions about what technology to include in this initiative. In addition to reliability and performance improvements, consider what user-driven features may benefit your facility.
Ethernet Communication

Station Upgrade
Experience the Benefits of Modernization
- Improved system uptime
- Fewer alarms
- Less time maintaining the system
- Reduced calls from users
- Improved clinical staff satisfaction
- Reduced spend for spare parts
Software Upgrade
Touchscreen Panel

Secure Content Tracking
The addition of content tracking functionality is primarily driven by inpatient pharmacies. There are a variety of tube system enhancements to consider when trying to achieve greater traceability of medication order delivery.
Xpress™ Transport
Enhanced Carrier Management
- Transaction Recovery: Automatic delivery of a carrier after a system shutdown.
- Inventory Management: Automated carrier inventory associates carriers with a “home” station, eliminating the need to cycle count.
- Condition Monitoring: The system can track how often a carrier is utilized and trigger a notification that preventive maintenance should be performed.
- Carrier/Station Association: Developed with end users in mind, this feature enables hospitals to assign carriers to a certain location, such as the pharmacy or the lab. This logic can, for example, prevent cross-contamination of carriers designated for specific payloads
Case Study: Children's Hospital of Alabama
Improving Throughput Via Pneumatic Tube System Upgrades
Background
- Frequent system downtime
- Calls and complaints from clinical users

Solution
To ensure the tube system is operating at peak productivity, TransLogic recommended the facility upgrade to the latest hardware and software. The hospital also chose to add chain-of-custody features to improve traceability and accountability of deliveries.
System enhancements included:
- Upgrade to new software
- Intuitive touchscreen panels
- RFID delivery tracking
- Secure badge access
Results
After upgrading their tube system, Children's of Alabama experienced several benefits:
- Improved system uptime
- Experienced fewer alarms
- Spent less time proactively maintaining the system
- Reduced calls from users about the system
- Satisfied their clinical staff with the system
- Spent less on spare parts
Conclusion
References
- Massachusetts Board of Registration in Pharmacy. (n.d.). Reasons for prescription errors.
- HCAHPS 2.0 Adult Core Questionnaire - hcahpsonline.org. (n.d.). Retrieved June 12, 2017
- Daly, C. C., MS, RN, NP. (2002, February 4). Missing Meds. Retrieved February 22, 2017
- Deaths/Mortality, 2005, National Center for Health Care Statistics at the Centers for Disease Control
- O’Neil, D. P., Sautman, H. L., & Hatfield, C. J. (2014, July). Missing Doses: A System at Fault. Retrieved February 22, 2017
- Flynn, E. A., Barker, K. N., Gibson, J. T. et al. (1999). Impact of interruptions and distractions on dispensing errors in an
ambulatory care pharmacy. American Journal of Health-System Pharmacists, 56, 1319-1325 - TechValidate. (2017, April). [Survey of 59 hospitals, TV ID 852-D2C-C46]. Unpublished raw data.
